Background: Children with sickle cell disease (SCD) often experience pain and have impaired physical functioning. Patient Reported Outcomes Measurement Information System (PROMIS) tools have previously been shown to be valid and responsive to varied states of health for children with SCD. However, there is limited understanding of the trend of patient-reported outcomes (PROs) over time and the factors associated with this trend and time-dependent changes. The objective of this study was to determine the longitudinal trends in physical functioning domains in children with SCD over a three-year time period and identify factors associated with worse PROs.
Methods: Our study included a convenience sample of children with SCD recruited from a tertiary care facility during 2017 - 2020. Eligible children with SCD to self-report PROs were 8 years and older and cognitively capable. Validated PROMIS measures were used to assess fatigue, physical stress experience, strength impact and functioning/mobility over time. The PRO questionnaires were administered every 6 months (with time windows to facilitate completeness of data) for three years to obtain longitudinal data. In addition, we collected clinical data including disease management strategy (hydroxyurea use, chronic transfusion), pain medication, prior acute care use for pain (3 years at baseline and 6 months at follow-up) disease complications (overt stroke, acute chest syndrome, priapism) and other comorbidities. Generalized Estimating Equations with patients as clusters were used to determine changes in PROs over time. This model used compound symmetry covariance structure to account for correlations over time and was adjusted for age and other clinical data. Stepwise regression model was used to identify the significant variables associated with PROs.
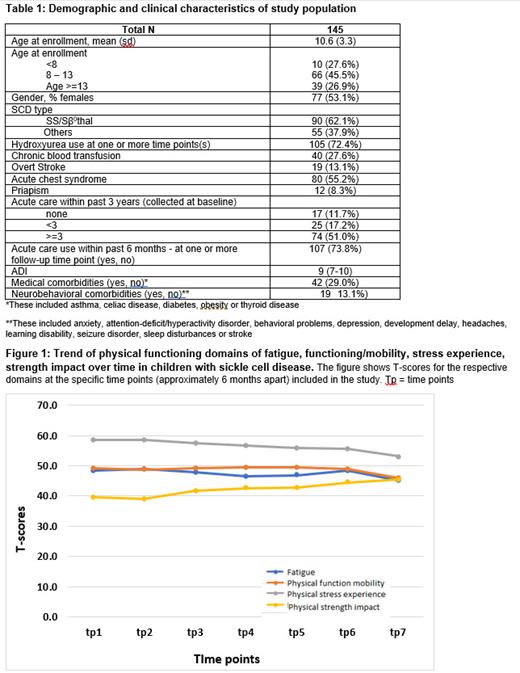
Results: We recruited 170 children with SCD into our study. Of these, 145 (85.3%) had self-report PRO data for more than one time point. The mean age of the cohort was 10.6 (SD 3.3) years, 53.1% were female. Table 1 shows the demographic and clinical characteristics of our study population. The average T-score for fatigue, physical functioning/mobility, stress experience and strength impact were 47.9, 49.1, 57.2 and 41.5 respectively. Figure 1 shows the unadjusted T-scores over time for each of the listed domains. The regression models showed there were no significant changes in scores for fatigue and physical function mobility over time. However, the stress experience [β (time in months) = -0.13 (95% CI = -0.20 - - 0.07), p-value <0.0001] and strength impact B estimate [β (time in months) = 0.13 (95% CI = 0.08 - 0.18), p-value <0.0001] improved over time. Age at enrollment was significantly associated with strength impact where older kids had a higher strength impact [β (age) = 0.49 (95% CI = 0.15 - 0.83), p = 0.005]. However, age was not associated with any of the other physical functioning domains. Disease severity at baseline, as determined by acute care use in the past three years, was significantly associated with stress experience [β (3 or more acute care visits for pain vs none) = 6.32 (95% CI = 1.71 - 10.93), p-value =.007] and fatigue [β (3 or more acute care visits for pain vs none) = 5.31 (95% CI = 0.95 - 9.66), p-value =.03]. The extent of acute care use within 6 months at follow-up time points was significantly associated with worse fatigue [β (acute care for pain within past 6 months) = 2.19 (95% CI = 0.19 - 4.20), p-value = 0.03] and physical functioning/mobility [β (acute care for pain within past 6 months)=-1.76 (95% CI = -3.24 - - 0.28), p-value = 0.02].
Conclusions: Fatigue and functioning/mobility did not change over time in children with SCD. There were slight improvements in stress experience and strength impact, but the clinical significance of these improvements is unknown. Disease severity, as measured by acute care use at baseline, was significantly associated with worse physical health across all domains.
Disclosures
No relevant conflicts of interest to declare.